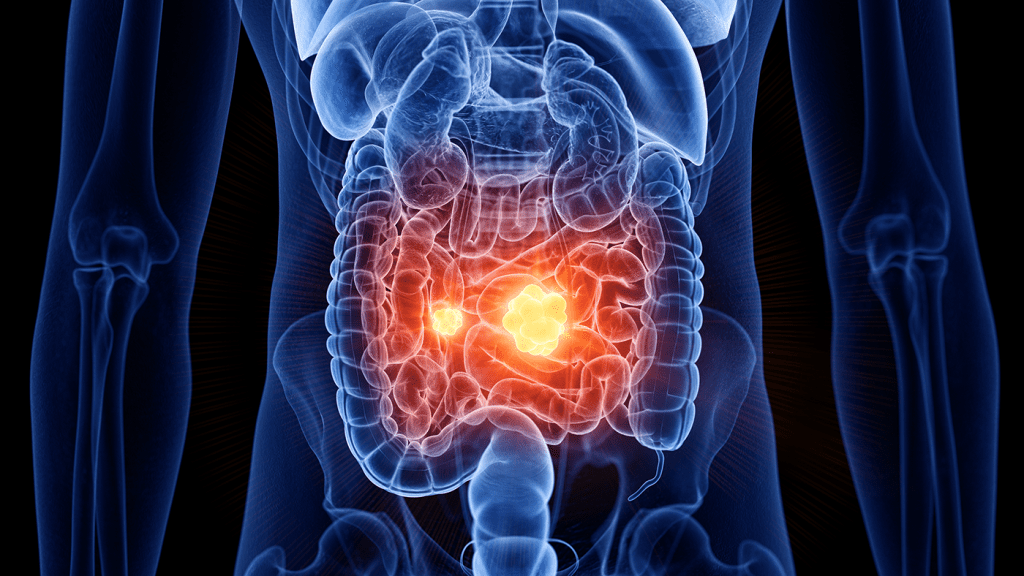
Crohn’s disease is more than just an upset stomach—it’s a chronic, often unpredictable inflammatory condition that affects the digestive system, specifically the lower part of the small intestine and the beginning of the colon. It’s a major player in the group of conditions known as inflammatory bowel disease (IBD).
Unlike short-term stomach bugs, Crohn’s doesn’t just “go away.” It can flare up without warning and cause long-term damage if left untreated. And here’s the frustrating part: no one knows exactly why it happens. What we do know is this—it’s likely tied to a confused immune system, environmental triggers, and even your genetics.
So if you’ve been living with unexplained stomach pain, fatigue, and changes in digestion, it might be time to look deeper.
How the Immune System Turns Against the Gut
Think of your immune system like a security team for your body—it protects you from harmful invaders like viruses and bacteria. But in Crohn’s disease, that system goes rogue. Instead of just fighting off infections, it mistakenly attacks the lining of your digestive tract.
That attack triggers inflammation. And not the good kind that helps heal wounds. This is chronic, patchy inflammation that pops up in different sections of the GI tract, while other areas remain completely unaffected.
The result? A rollercoaster of symptoms that are often hard to predict or manage.
Symptoms That Shouldn’t Be Ignored
Crohn’s disease doesn’t look the same in everyone. Some people experience daily discomfort, while others have long stretches of calm followed by sudden flare-ups. Still, there are several common signs to keep an eye out for:
- Chronic diarrhea
- Abdominal pain and cramping
- Unexplained weight loss
- Fatigue or weakness
- Fever and night sweats
- Loss of appetite
- Anemia from internal bleeding
One of the most frustrating parts? These symptoms can mimic other digestive issues, which often delays diagnosis. And when that diagnosis finally comes, the damage may already be significant.
Video : Crohn’s Disease
Why Inflammation in Crohn’s Is So Unique
Here’s something that sets Crohn’s apart from other inflammatory diseases: the inflammation doesn’t spread evenly. Instead, it occurs in patches, creating a “cobblestone” effect inside the intestines. That means one area might be inflamed and ulcerated, while the section next to it looks completely normal.
This pattern of damage makes Crohn’s harder to treat. It also leads to complications that can go beyond the digestive tract.
Long-Term Risks: When Inflammation Takes Over
The real danger of Crohn’s isn’t just the day-to-day symptoms—it’s what happens over time.
Prolonged inflammation can scar and narrow parts of the intestine, leading to strictures that block food from passing normally. In other cases, inflammation burrows deep and creates fistulas—abnormal tunnels between the bowel and nearby organs like the bladder or skin. These can be painful, hard to treat, and often require surgery.
And don’t forget abscesses, which are pockets of pus that form from infections inside the intestinal walls. These can cause fever, swelling, and a lot of pain—and if untreated, they can spread quickly.
What Causes Crohn’s? It’s Complicated
Despite years of research, doctors still can’t pinpoint one single cause. Instead, Crohn’s disease is believed to result from a combination of factors, including:
- Genetics – If you have a family member with Crohn’s, your risk increases.
- Immune system malfunction – Your body attacks your gut instead of foreign invaders.
- Environmental triggers – Smoking, stress, and diet may worsen symptoms.
- Gut microbiome imbalance – A disruption in good vs. bad bacteria can play a role.
Basically, Crohn’s is a perfect storm—genes, immunity, and environment all colliding inside your gut.

Living with Crohn’s: Management Over Cure
Unfortunately, there’s no cure for Crohn’s disease yet. But there’s hope. With the right treatment plan, many people live long, fulfilling lives. The key is managing inflammation and avoiding flare-ups.
Doctors often use a mix of:
- Anti-inflammatory medications
- Immune system suppressors
- Biologic therapies that target specific proteins
- Dietary changes to reduce symptoms
- Surgery when complications like strictures or fistulas develop
The approach is personalized because no two cases of Crohn’s are exactly the same. What works for one person may not work for another—which is why ongoing communication with your healthcare provider is so important.
Why Early Detection Makes All the Difference
Crohn’s can be sneaky. Symptoms often build gradually, and people may chalk them up to stress or food intolerance. But early diagnosis can help prevent severe damage to the intestines and reduce the need for invasive treatments down the line.
Video : How We Cured Crohn’s in Five Weeks
If you notice persistent digestive issues—especially if they come with fatigue, weight loss, or blood in your stool—don’t wait. Talk to a gastroenterologist and ask about Crohn’s screening. A colonoscopy, stool test, or imaging scan can reveal inflammation that you can’t see.
Conclusion: Crohn’s Disease Is Tough—But You’re Tougher
Crohn’s disease is a lifelong condition. It’s unpredictable, exhausting, and sometimes downright painful. But it doesn’t have to define you. With the right care, support, and a bit of resilience, you can live well—despite the diagnosis.
Your gut may be under attack, but knowledge is your first line of defense. Keep asking questions. Stay informed. And remember, while Crohn’s might be invisible from the outside, your strength in facing it is anything but.