A recent medical study has sparked concern after revealing that anal cancer is quietly on the rise, especially among a group of people not typically considered at high risk. The findings, presented at Digestive Disease Week (DDW) 2025, are now prompting a renewed focus on awareness, prevention, and early detection.
If you think anal cancer only affects a small portion of the population, you might want to think again. The numbers are climbing—and fast.
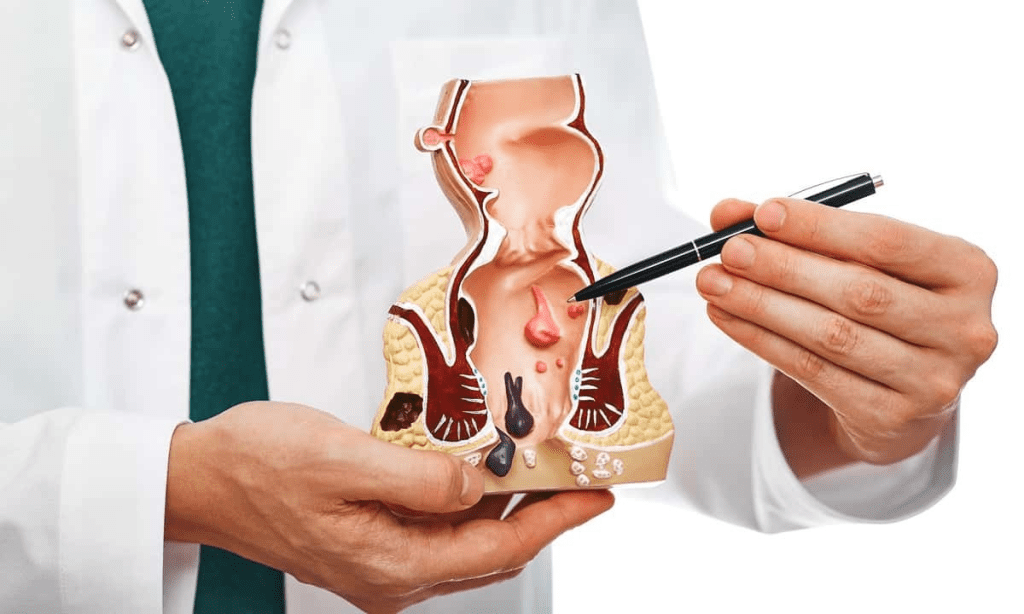
What Is Anal Cancer and Why Is It So Often Overlooked?
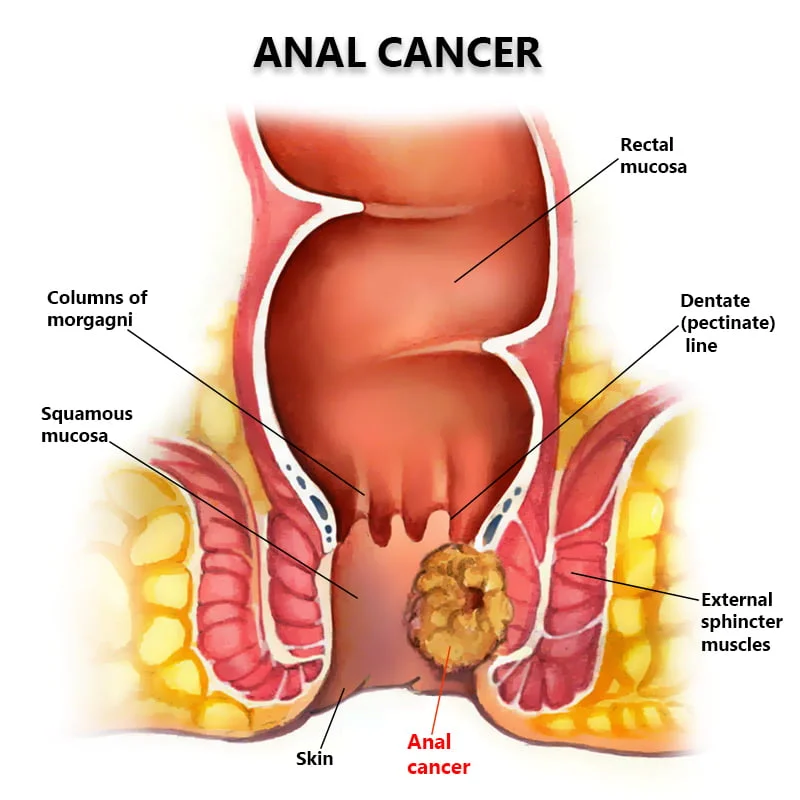
Anal cancer is a rare form of cancer that affects the anus, the area where your digestive tract ends and exits the body. It’s not widely talked about, partly because it’s often mistaken for less serious issues like hemorrhoids or fissures.
That’s a big part of the problem. The symptoms of anal cancer can appear minor at first, including:
- Bleeding from the bottom
- Pain or itching around the anus
- Lumps inside or around the anal area
- Mucus discharge
- Irregular bowel movements
Because these signs often mimic other non-threatening conditions, many people don’t seek medical attention right away—leading to late diagnoses and more complicated treatments down the line.
The Surprising Demographic Most at Risk
Here’s what caught researchers off guard. According to data collected between 2017 and 2021, white and Hispanic women over the age of 65 are experiencing the fastest increase in anal cancer cases.
This is a major shift from the typical risk profile. Traditionally, other groups were considered higher risk due to immune conditions or behavioral factors. But now, the spotlight is shifting to a different demographic entirely.
Video : Doctor explains SYMPTOMS OF ANAL CANCER – plus risk factors, diagnosis and treatment
White women over 65 saw a 4.43% increase in cases, while Hispanic women in the same age group experienced a 1.7% rise. Overall, cases increased by 2.9% for women and 1.6% for men during the study’s five-year window.
Lead researcher Dr. Ashley Robinson believes part of this trend may be linked to the rollout of the HPV vaccine—or more accurately, the fact that many older women missed out on it.
HPV: The Hidden Culprit Behind Anal Cancer
The primary cause of anal cancer is human papillomavirus, commonly known as HPV. It’s an extremely common virus transmitted through skin-to-skin contact, especially during sexual activity.
In most people, the immune system clears the virus naturally. But in some, HPV can linger and lead to cell changes that eventually become cancer.
The HPV vaccine is a powerful preventative tool. Unfortunately, many of the women now being diagnosed with anal cancer were already adults when the vaccine first became available. That timing left them unprotected.
These findings are a strong reminder of the vaccine’s value—and the importance of catching up for those who may have missed it.
Why Screening Isn’t Catching It Early

One of the biggest challenges with anal cancer is that there’s no national screening program. Unlike breast or cervical cancer, there’s no widely-used test for early detection.
According to Cancer Research UK, this is largely because a standardized, accurate screening test doesn’t exist yet for this type of cancer. That means prevention and awareness are even more important.
Without a test, recognizing early symptoms and knowing your risk factors could make the difference between catching it early—or too late.
The Case for Widening HPV Vaccine Access
Vaccination isn’t just for teens anymore. While the standard recommendation is to vaccinate children aged 12 to 13, catch-up vaccines are available for people up to age 25, and in some cases even older with doctor approval.
The key is education. Many adults still don’t realize how effective the HPV vaccine is in preventing multiple types of cancer, including anal cancer.
Dr. Robinson emphasizes the importance of making the vaccine more accessible and promoting it to groups who might not see themselves at risk—especially older adults. She also highlights the need for medical professionals to stay up to date with the evolving screening recommendations and to think outside traditional risk profiles.
So, What Can You Do?
Start by being informed. If you’re in your 50s, 60s, or older and you’ve never received the HPV vaccine, talk to your doctor. You may still be eligible, and even partial protection is better than none.
If you experience unusual symptoms around your anal area—especially bleeding, lumps, or discomfort that won’t go away—get it checked out. Don’t assume it’s just hemorrhoids.
And if you’re a parent or guardian, ensure your children receive the HPV vaccine at the recommended age. It’s one of the most effective tools we have to stop several cancers before they ever start.
Why This Study Matters More Than You Think
The takeaway is simple, but powerful. Anal cancer is increasing, and not in the groups we’d traditionally expect. That’s why public health messaging needs to shift. We can’t assume only younger or immunocompromised people are at risk. The data proves otherwise.
Video : Anal Cancer: Should Screening be Routine?
It’s time to widen the conversation, support targeted screening efforts, and empower more people with the knowledge they need to protect themselves.
Share the Knowledge, Save a Life
This isn’t just another health headline. It’s a wake-up call.
If this article helped you understand the risks better, don’t keep it to yourself. Share it with the people you care about—your parents, siblings, friends, and anyone else who might fall into the new risk categories.
Because when it comes to cancer, knowledge really is power. And in this case, spreading the word could quite literally save lives.