What Is Insulin Resistance?
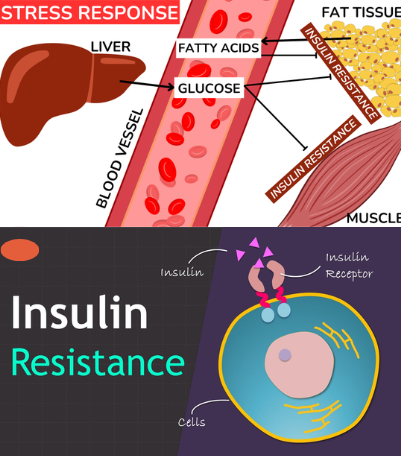
Insulin resistance happens when your body’s cells don’t respond properly to insulin, the hormone that helps move glucose (sugar) from your blood into your cells for energy. As a result, your pancreas works overtime, producing more insulin to keep blood sugar levels stable. Over time, this imbalance can lead to prediabetes, type 2 diabetes, and other serious health issues. Think of it like a key (insulin) struggling to unlock a door (your cells)—when the lock doesn’t work well, sugar stays outside in the bloodstream.
What Causes Insulin Resistance?
Insulin resistance develops from a mix of lifestyle factors, genetics, and health conditions. The main causes include:
- Excess weight, especially belly fat – Abdominal fat produces hormones that interfere with insulin function.
- Sedentary lifestyle – Lack of physical activity reduces your body’s ability to use glucose effectively.
- Unhealthy diet – Diets high in refined carbs, sugary drinks, and processed foods spike blood sugar repeatedly.
- Hormonal changes – Conditions like polycystic ovary syndrome (PCOS) increase insulin resistance risk.
- Genetics and family history – Having relatives with diabetes raises your chances.
- Chronic stress and poor sleep – Both affect hormone balance and blood sugar control.
These factors combined create a perfect storm, pushing the body toward resistance.
Signs and Symptoms of Insulin Resistance
Insulin resistance often creeps in silently, but certain symptoms can serve as early red flags:
- Constant fatigue or low energy.
- Unexplained weight gain, especially around the waist.
- Increased hunger and cravings for sweets.
- Difficulty losing weight despite effort.
- High blood pressure and cholesterol levels.
- Dark, velvety patches on the skin (acanthosis nigricans).
- Brain fog or difficulty concentrating.
Because these symptoms can mimic other conditions, many people don’t realize they have insulin resistance until it progresses.
Video : What Is Insulin Resistance?
Why Insulin Resistance Matters
Ignoring insulin resistance can set the stage for bigger health problems, including:
- Prediabetes and type 2 diabetes – Chronic high blood sugar damages blood vessels and organs.
- Heart disease – Insulin resistance is linked with high blood pressure, high triglycerides, and low HDL (“good” cholesterol).
- Non-alcoholic fatty liver disease (NAFLD).
- Increased risk of stroke and kidney disease.
Think of insulin resistance as the first domino in a chain reaction of health problems. Addressing it early can stop the rest from falling.
How Insulin Resistance Is Diagnosed
Doctors use a combination of tests to confirm insulin resistance:
- Fasting blood sugar – Elevated levels suggest poor glucose control.
- Hemoglobin A1C test – Measures average blood sugar over three months.
- Fasting insulin test – Detects high insulin levels.
- HOMA-IR calculation – A formula combining insulin and glucose levels to measure resistance.
These tests help determine whether lifestyle changes or medical interventions are needed.
Lifestyle Changes to Improve Insulin Sensitivity
The good news? Insulin resistance can often be reversed with consistent lifestyle changes:
- Eat a balanced diet – Focus on whole foods, fiber-rich vegetables, lean proteins, and healthy fats. Limit sugary drinks and refined carbs.
- Exercise regularly – Both aerobic exercise (walking, cycling) and strength training improve insulin sensitivity.
- Lose excess weight – Even a 5–10% reduction in body weight can make a big difference.
- Get quality sleep – Aim for 7–9 hours nightly to restore hormone balance.
- Reduce stress – Yoga, meditation, or breathing exercises lower stress hormones that interfere with insulin.
- Stay hydrated – Drinking enough water helps the body regulate blood sugar.
These steps are like fine-tuning your body’s engine—making it run more efficiently with less strain.
Medical Treatment for Insulin Resistance
In some cases, lifestyle changes may not be enough. Doctors may prescribe:
- Metformin – A common drug that lowers blood sugar and improves insulin sensitivity.
- Medications for weight loss – Especially for those struggling with obesity.
- Cholesterol and blood pressure medications – To reduce cardiovascular risks linked with insulin resistance.
These are often used alongside, not instead of, lifestyle changes.
Prevention: Protecting Yourself from Insulin Resistance
Preventing insulin resistance is easier than treating it. Key strategies include:
- Maintaining a healthy weight.
- Staying active daily.
- Choosing whole foods over processed ones.
- Avoiding smoking and limiting alcohol.
- Getting regular health checkups to monitor blood sugar and cholesterol.
It’s like building a protective shield—once it’s in place, it’s much harder for insulin resistance to break through.
Video : Mayo Clinic Explains Insulin Resistance
Conclusion: Taking Charge of Your Health
Insulin resistance may sound intimidating, but it’s not a life sentence. With awareness, smart lifestyle changes, and medical support when needed, you can improve your body’s response to insulin and prevent long-term complications. The key is early action—because the sooner you address it, the easier it is to restore balance. By fueling your body wisely and keeping active, you’re not just preventing insulin resistance—you’re investing in a healthier, stronger future.


