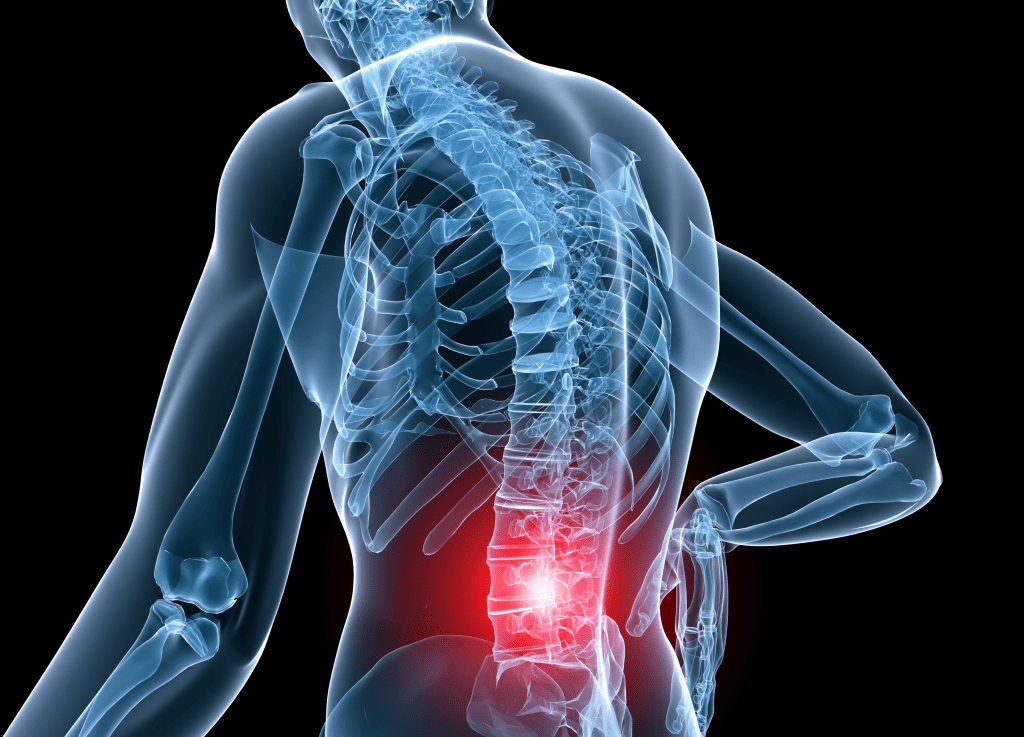
If you’ve ever battled chronic back pain, chances are you’ve heard about spine injections—epidural steroid shots, nerve blocks, or maybe even radiofrequency ablation. They’re marketed as quick fixes, the kind of procedures that promise to knock out pain and help you “get your life back.” But what if we told you that recent evidence suggests they don’t actually work any better than a placebo?
That’s right. According to a major review from a panel of international experts published in The BMJ, these commonly used spine injections offer little to no meaningful pain relief. And here’s the kicker—they can be expensive, carry risks, and may not be worth the trouble for most people. Let’s break it down.
The Epidemic of Chronic Back Pain

Chronic back pain isn’t just annoying—it’s a global health crisis. Roughly 1 in 5 adults aged 20 to 59 deals with some form of persistent spine pain. And for older adults? The numbers climb even higher. In the U.S. alone, treating low back and neck pain cost $134.5 billion in 2016, making it the single biggest contributor to healthcare spending.
So, it makes sense that people desperately seek relief. The trouble is, not all treatments are created equal, and spine injections might be one of the biggest medical myths still hanging around in modern practice.
Spine Injections: The Promise vs. the Reality
For years, treatments like epidural steroid injections, nerve blocks, and radiofrequency ablation have been used to relieve chronic spine pain by interrupting nerve signals. On the surface, they sound like medical magic: target the pain directly and shut it down.
But here’s the reality, straight from a rigorous scientific review: these injections work no better than sham procedures. That’s right—people receiving placebo treatments reported about the same level of pain relief as those getting real injections.
The review looked at 13 of the most common interventional procedures and found that even the best-case scenarios didn’t show meaningful, long-lasting improvement in pain.
Video : Epidural corticosteroid injection for management of chronic lower back pain
The Panel’s Verdict: Strongly Against
This isn’t just one person’s opinion—it’s a formal recommendation from an international panel of clinicians, chronic pain patients, and researchers who used the highly respected GRADE framework to assess the evidence.
Their conclusion? Strongly recommend against using spine injections for chronic back pain that isn’t related to cancer, infection, or inflammatory arthritis.
That includes:
- Local anesthetic injections
- Steroid-only injections
- Epidural combinations of both
- Radiofrequency ablation, with or without anesthetics or steroids
Why the strong stance? Because the procedures are costly, pose a small but real risk of harm, and—most importantly—don’t deliver significant benefits. According to the panel, almost all well-informed patients would likely choose to skip these procedures once they knew the facts.
Why Do These Injections Still Happen?
You might be wondering, if the evidence is this clear, why are these injections still so common? The answer lies in medical culture, patient expectations, and yes—money.
Many healthcare systems and insurance companies continue to fund these procedures, and some doctors are still trained to offer them as first-line solutions. It’s hard to change long-standing habits in medicine, especially when patients expect immediate action.
But as Dr. Jane Ballantyne from the University of Washington writes in a related editorial, “the more the evidence fails to support the widespread use of these injections, the less inclined healthcare systems will be to fund them.”
In other words: change is coming.
Where Do We Go From Here?
Here’s the good news—this isn’t the end of the road for treating chronic back pain. In fact, this new research might be the beginning of a better approach. Instead of defaulting to injections, we need to think more broadly and more creatively about non-invasive, patient-centered care.
That includes:
- Physical therapy
- Mindfulness and cognitive-behavioral therapy
- Exercise-based rehabilitation
- Multidisciplinary pain management programs
Not only do these approaches carry fewer risks, but they may actually offer longer-lasting relief—and they empower patients to take control of their recovery.
Why Evidence-Based Pain Care Matters
Let’s face it—when you’re in pain, you want relief now. But real solutions aren’t always the fastest or flashiest. What we’re seeing with this new spine injection research is a much-needed shift in perspective.
Pain treatment isn’t just about doing something—it’s about doing the right thing. And sometimes, that means not doing something, especially when the evidence says it’s ineffective.
It’s also worth noting that ongoing research may change things in the future. Some procedures that currently have low-certainty evidence might eventually prove effective with better trials. But until then, the responsible choice is to focus on treatments that actually work—not ones that just sound good.
So What Should You Do If You Have Chronic Back Pain?
Start by talking to your doctor about non-interventional treatment options. Ask for a plan that includes movement, education, and a long-term strategy—not just a short-term fix.
Video : Back Pain Relief – Lumbar Epidural
Be cautious of promises that sound too good to be true. And don’t be afraid to get a second opinion, especially if spine injections are being pushed without a clear explanation.
Remember, your time, your money, and your health matter. You deserve a treatment plan based on solid evidence, not outdated habits.
Conclusion: It’s Time to Rethink Chronic Pain Treatment
Spine injections for chronic back pain might look appealing on the surface, but the science says otherwise. With minimal benefit, high costs, and potential risks, it’s no wonder experts are now urging doctors and patients to reconsider their use.
This isn’t about denying treatment—it’s about finding better ones. Chronic pain is real, and managing it requires a thoughtful, evidence-based approach. The future of pain care lies not in the syringe, but in personalized, holistic strategies that empower people to heal.
The bottom line? When it comes to spine injections, it’s time to press pause and look for smarter, safer solutions.