A new, more dangerous variant of mpox, formerly known as monkeypox, has been identified in the United Kingdom for the first time. The disease, which can cause debilitating symptoms and even lead to hospitalization, was detected in a UK patient after they returned from a trip to Africa. As health officials rush to contain any potential spread, doctors are urging people to stay vigilant and be aware of the symptoms of this “horrendous” disease that left one previous patient unable to move or eat.
What Is Mpox and How Did It Reach the UK?
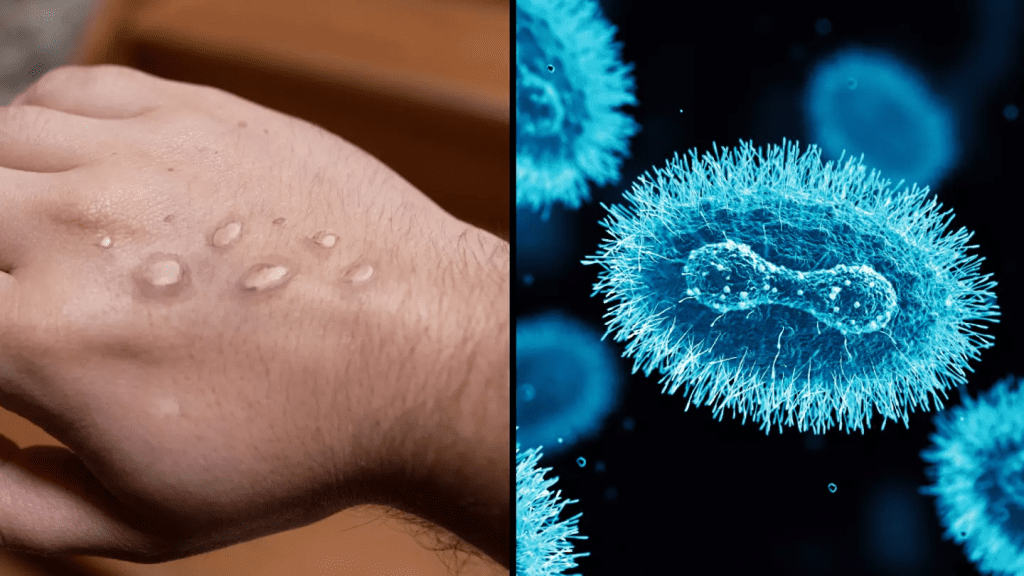
Mpox is a viral disease that was historically associated with small, isolated outbreaks in Africa. However, global transmission rates have increased, and in 2022, the World Health Organization (WHO) declared mpox a global health emergency. The disease, caused by the mpox virus, can lead to painful skin lesions, high fever, and severe fatigue. While past outbreaks were generally mild, the recent detection of a new variant, Clade 1b, raises concerns due to its potentially severe symptoms and higher rate of spread.
The UK Health Security Agency (UKHSA) confirmed the presence of this variant, known as Clade 1b, which differs from the Clade II variant that has circulated in the UK since 2022, primarily among certain at-risk groups. This latest case is believed to have originated in Africa, where Clade 1b is more prevalent.
Symptoms of Mpox: What to Look Out For
Dr. John Burke, Chief Medical Officer of AXA Health, has identified four main symptoms to be mindful of, noting that these symptoms are often mistaken for other infectious illnesses, such as chickenpox.
- Blister-like Rash Across the Body: The most notable symptom of mpox is a rash that resembles blisters or sores. These lesions typically appear on the face and body and can be painful. The rash often starts small but can spread quickly, causing severe discomfort.
- High Fever and Chills: Mpox often triggers a high fever, which may be accompanied by chills. This fever can be severe, often leading to night sweats and an overall feeling of weakness.
- Flu-like Aches and Pains: Infected individuals may experience intense body aches, including muscle soreness, back pain, and headaches. Fatigue and a sense of exhaustion are also common.
- Swollen Lymph Nodes: Another telling sign of mpox is the presence of swollen lymph nodes, which can be painful and may persist even after other symptoms begin to subside.
These symptoms may start out feeling like the flu but can escalate quickly. Dr. Burke emphasizes the importance of seeking medical advice if someone experiences these symptoms, particularly if they’ve traveled to Africa recently or have been in contact with a known case.
The Patient’s Experience: A Firsthand Account of Mpox
One London resident, Harun Tulunay, shared his harrowing experience with mpox in 2022 during a prior outbreak. Harun’s ordeal began with a high fever and severe muscle pain, which quickly worsened. His symptoms progressed to include painful lesions and scars all over his body. He recounted, “After two weeks of horrendous high fever and pain, I wasn’t able to move or drink or eat anymore.” Harun’s symptoms became so intense that he required hospitalization.
After his recovery, Harun received the mpox vaccine, which offers protection against future variants of the virus. He has since become an advocate for global vaccine distribution, especially in regions of Africa where the virus is spreading most aggressively.
How Mpox Is Transmitted and Who Is at Risk
Mpox spreads primarily through close physical contact with infected individuals. This includes direct contact with bodily fluids, respiratory droplets, and skin lesions. While it was initially contained to certain regions, recent travel and international mobility have allowed the virus to spread beyond its traditional boundaries.

The current mpox variant, Clade 1b, is still considered low-risk for the general UK population. However, the virus remains a concern for travelers to affected areas, healthcare workers, and those in close contact with infected individuals. The UKHSA has initiated contact tracing to monitor and reduce the risk of further transmission.
Public Health Measures and the UK’s Response to Mpox
Upon confirming the new variant, the UK Health Security Agency took immediate steps to prevent its spread. The infected individual was isolated and transferred to the Royal Free Hospital High Consequence Infectious Diseases Unit in London. UKHSA and NHS officials are closely monitoring anyone who may have come into contact with the infected patient to reduce transmission risk.
Professor Susan Hopkins, Chief Medical Adviser at UKHSA, emphasized the importance of the agency’s surveillance efforts, stating, “It is thanks to our surveillance that we have been able to detect this virus. The risk to the UK population remains low, and we are working rapidly to trace close contacts.” Health authorities are also investigating how the patient contracted the infection and are looking into other potential cases.
Prevention and Vaccine Availability for Mpox

Currently, there is an effective vaccine available for mpox, which can help prevent infection or lessen the severity of symptoms. The vaccine was initially reserved for high-risk groups during previous outbreaks but is now being administered more broadly in response to increasing cases. Vaccination is especially important for healthcare workers, people who frequently travel to regions with high mpox transmission rates, and those with known exposure to the virus.
Dr. Burke reassures that while mpox can be severe, many people recover within a few weeks without the need for extensive treatment. “If you do contract the virus, it is usually mild, and most people recover within a few weeks,” he says. Nevertheless, vaccination remains a vital tool in preventing severe cases, particularly with the emergence of Clade 1b.
The Importance of Early Detection and Medical Consultation
Given the similarities between mpox symptoms and those of other common infections like chickenpox, early detection can be challenging. Dr. Burke advises anyone experiencing mpox symptoms, particularly after travel, to seek professional medical advice immediately. Identifying the virus early allows for timely isolation and treatment, reducing the risk of complications and helping prevent transmission.

In cases where mpox progresses to severe symptoms, hospitalization may be required to manage pain and prevent dehydration. As seen in Harun’s case, symptoms can worsen rapidly, and medical support may be necessary.
Conclusion: Staying Informed and Vigilant Against Mpox
The recent detection of a new mpox variant in the UK is a reminder of the importance of vigilance, especially as new strains of viruses emerge globally. Mpox, while generally mild, can lead to severe symptoms and hospitalization if left untreated. With early detection, access to vaccines, and preventive measures, the risk of spread can be minimized.
By staying informed about the symptoms and understanding the importance of medical consultation and vaccination, individuals can help protect themselves and their communities from this “horrendous” disease. The UK’s health agencies are working tirelessly to monitor and contain mpox, but personal awareness and caution remain critical in managing this evolving public health threat.