Cancer research is entering a new era — one where the immune system is no longer a passive bystander, but a precision-trained warrior. Scientists have developed a groundbreaking new type of cancer vaccine that teaches your immune system to recognize and destroy tumor cells. Sounds futuristic? It’s happening now — and early results suggest it might be one of the most promising tools in the fight against one of the deadliest cancers of all: pancreatic cancer.
Drawing on the same mRNA technology used in COVID-19 vaccines, researchers are now leveraging personalized mRNA-based vaccines to help cancer patients live longer, healthier lives. Here’s everything you need to know about this revolutionary treatment, how it works, what we’ve learned so far, and why it’s both incredibly hopeful — and still in its early days.
Understanding mRNA Vaccines and Their Role in Cancer Immunotherapy
You probably heard a lot about mRNA during the pandemic, but this technology wasn’t just designed for viruses. At its core, mRNA (messenger RNA) carries instructions to your cells — telling them what proteins to make. In vaccines, that message trains the immune system to recognize harmful targets.
In cancer treatment, this message can be customized to match the unique fingerprints of a patient’s tumor. These fingerprints, known as neoantigens, are specific mutations only found on cancer cells. By encoding these into a vaccine, doctors can teach the immune system to recognize and attack cancer — just like it would a virus.
How the mRNA Cancer Vaccine Works
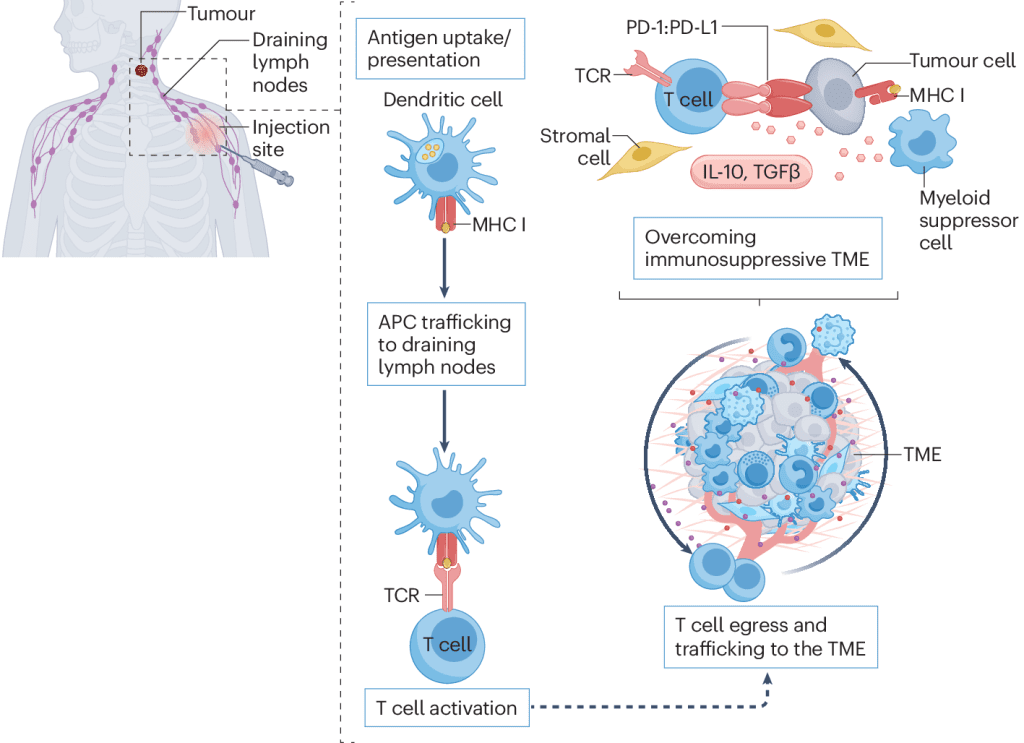
Think of it like this: your immune system is a security force, but sometimes it doesn’t recognize the threat. Cancer cells are sneaky — they disguise themselves as normal cells. The mRNA vaccine removes that disguise.
Here’s the simplified step-by-step:
- A sample of the patient’s tumor is collected and genetically profiled.
- Scientists identify the neoantigens (unique mutated proteins) on those cancer cells.
- They create a custom mRNA vaccine that teaches the immune system to detect and attack anything showing those markers.
- Once injected, the vaccine stimulates T-cells to seek and destroy tumor cells with those exact features.
This method doesn’t just treat symptoms — it trains the body to fight the root cause.
Video : Cancer-busting vaccines are coming: here’s how they work
Promising Results from Early Clinical Trials
One of the most exciting examples of this technology is currently being studied in patients with pancreatic ductal adenocarcinoma — a brutal form of cancer with a historically poor survival rate. In a recent 2023 trial led by Memorial Sloan Kettering Cancer Center in collaboration with BioNTech, researchers gave personalized mRNA vaccines to patients who had surgery to remove their tumors.
Here’s what they found:
- Around half of the patients developed a strong immune response after vaccination.
- Those who responded well were significantly less likely to experience relapse in the short term.
- The vaccine was well-tolerated and combined with standard treatments like chemotherapy.
It’s still early, but these results are incredibly promising for a cancer type that rarely triggers strong natural immune reactions.
What Makes Pancreatic Cancer So Difficult to Treat
Pancreatic cancer is notoriously aggressive. It’s often diagnosed late, doesn’t respond well to traditional treatments, and has one of the lowest five-year survival rates of any major cancer. The biggest challenge? It hides from the immune system.
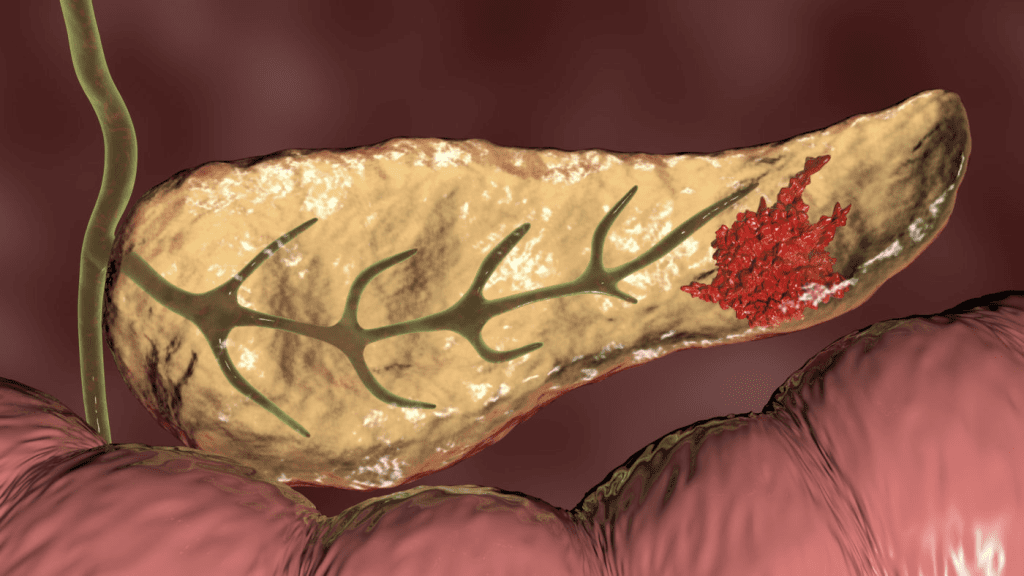
That’s why this new vaccine approach is such a game-changer. Instead of bombarding the body with toxic treatments, it activates and sharpens the immune response — precisely targeting the tumor, especially in the early stages after surgical removal.
The Hype vs. The Reality: Can This Really Add “Decades” to Life?
Let’s address the bold headlines: can this vaccine add decades to a patient’s life?
Here’s the honest take — maybe, but we’re not there yet.
Right now, the results show that this treatment can delay relapse and potentially extend survival, especially for patients who’ve had tumors surgically removed. That’s a huge step forward. But the sample sizes are small, and we don’t yet have long-term data to prove these results lead to decades of added life.
This doesn’t mean the science isn’t promising — it just means we need to stay grounded. The excitement is real, but so is the need for more trials, more patients, and more time.
Why Personalized Vaccines Aren’t an Instant Fix
As groundbreaking as this approach is, there are still hurdles to overcome:
- Time and cost: Each vaccine is personalized, requiring analysis of a patient’s tumor and weeks of development time.
- Access: Not every hospital or clinic has the capacity to provide this treatment right now.
- Limited to early-stage patients: So far, the best results have been seen in patients who already had their tumors removed surgically.
- Still in trial phase: The data is promising but not conclusive. We need Phase II and III studies to confirm everything.
This is cutting-edge science — and like anything new, it will take time before it becomes widely available.
Where This Treatment Is Headed Next
If ongoing trials confirm the early promise of these vaccines, we could be looking at a new standard of care for hard-to-treat cancers like pancreatic, melanoma, or even colon cancer. Researchers are also testing how these vaccines work when combined with checkpoint inhibitors (immune system “unleashers”) or standard chemotherapy, aiming to make the results even stronger.
More institutions are jumping in. Big names like Moderna, BioNTech, and major cancer centers are investing heavily in the future of personalized immunotherapy. That means access will improve, costs may go down, and survival rates could climb.
What Patients and Families Should Know Now
If you or a loved one has been diagnosed with pancreatic cancer, it’s worth asking your oncologist about current clinical trials. While these vaccines aren’t widely available yet, some major cancer centers are offering access through research programs.
Also, it’s important to combine hope with realism. This isn’t a miracle cure — but it is one of the most exciting developments in cancer research in years. It’s personalized, targeted, and rooted in science that’s already proven itself in other areas.
Video : Mayo Clinic Minute – How personalized vaccines target cancer tumors
Conclusion: A New Frontier in Cancer Treatment Is Emerging
A personalized mRNA cancer vaccine that helps the immune system find and fight tumor cells may sound like science fiction — but it’s becoming a reality. While we’re still early in this journey, the first steps are incredibly encouraging.
This approach doesn’t just aim to shrink tumors. It aims to train your own body to become a long-term guardian against cancer’s return.
As trials continue and more data emerges, we’ll better understand who benefits most, how to improve results, and how this fits into the broader cancer treatment landscape. But one thing is clear: the immune system has always had potential — and now, we’re finally unlocking it.