Lung cancer occurs when abnormal cells begin growing uncontrollably in lung tissue, disrupting respiratory function. Historically, the majority of lung cancer cases were tied to long-term tobacco use. But now, up to 20% of lung cancer cases are being diagnosed in people who have never smoked.
Let that sink in: 1 in 5 lung cancer patients never picked up the habit. In 2017 alone, there were over 1.57 million new male cases and 900,000 female cases globally. Even more striking, a subtype called adenocarcinoma is the most common among these non-smokers—especially women.
This shift has forced researchers to dig deeper and identify alternative culprits.
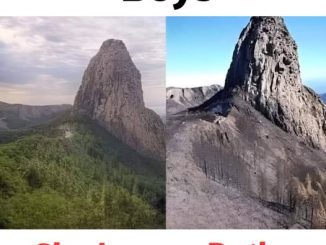
Air Pollution: The Silent Killer in Plain Sight

One of the biggest environmental threats hiding in plain sight is air pollution. Whether it’s the smog hovering over your city or the emissions from a nearby factory, the air you breathe can significantly affect your lung health—smoker or not.
Fine particulate matter—known as PM2.5 and PM10—is particularly dangerous. These tiny particles are small enough to lodge deep into your lungs, where they can trigger inflammation and potentially lead to cellular mutations. In heavily industrialized or urbanized areas, these particles often exceed safe limits, putting millions at risk daily.
Studies show that regions like East Asia and North Africa are seeing some of the highest rates of pollution-related lung cancer. But it’s not just a problem “over there.” If you live in a traffic-heavy city or near a manufacturing plant, you’re breathing in potential carcinogens every day.
Video : Why Is Lung Cancer in Non-smokers on the Rise?
Genetic Mutations: When It’s in Your DNA
Another key player in non-smoking lung cancer cases is genetics. Some people are simply born with a higher risk due to inherited mutations—especially in genes like EGFR, ALK, and KRAS. These mutations can spark uncontrolled cell growth even in the absence of environmental triggers like cigarette smoke.
What’s particularly dangerous is that these genetic drivers often go undetected until it’s too late. That’s why knowing your family history and undergoing regular medical screening is so important—especially if someone in your family has had lung cancer without smoking.
Lifestyle and Diet: More Powerful Than You Think
It’s easy to blame outside sources, but we can’t ignore how our personal habits contribute to cancer risk. While not as widely discussed, diet and lifestyle choices play a crucial role in either protecting or damaging our cellular health.

Here’s how:
- A diet low in fruits and vegetables means you’re missing out on essential antioxidants and vitamins that help your body repair damaged cells.
- Obesity and a sedentary lifestyle can lead to chronic inflammation—an underlying condition that’s linked to many types of cancer, including lung cancer.
In other words, if your body is constantly inflamed or poorly nourished, it becomes much easier for abnormal cells to grow unchecked.
Early Detection: The Best Chance at Beating the Odds
When it comes to cancer, early detection saves lives. Unfortunately, most lung cancer diagnoses—especially among non-smokers—happen at later stages when treatment becomes more difficult.
That’s why tools like low-dose computed tomography (CT) scans are so important. They can detect lung nodules before symptoms appear, giving patients a critical head start. However, because current screening guidelines mostly target smokers, many non-smokers never get screened at all—even if they’re at risk.
It’s time to shift that thinking. Researchers are now calling for new screening criteria that consider environmental exposure, genetic risk, and geographic location—not just smoking history.
The Bottom Line: It’s Not Just About Smoking Anymore
Lung cancer is no longer just a smoker’s disease. The numbers don’t lie: non-smokers are increasingly being diagnosed, and the causes are far more complex than once believed. Whether it’s polluted air, genetic mutations, or poor lifestyle habits, these silent threats are becoming louder and more dangerous by the year.
Video : Brevard County lung cancer survivor says she’s never smoked a day in her life
So what can you do?
- Be proactive about your health screenings, especially if you have a family history.
- Make lifestyle changes—like eating a balanced diet and staying active—to reduce inflammation and support immune function.
- Advocate for cleaner air policies in your community.
- Pay attention to unusual symptoms—even if you’ve never smoked.
Because when it comes to lung cancer, early awareness could be the difference between life and death. Let’s stop thinking of it as a smoker’s disease and start seeing it for what it really is: a public health crisis affecting us all.